This is the second post in my series on the “why” behind the new opioid guidelines. This series is meant to help understand why the changes in opioid prescribing occurred. Whether you agree with the changes or not, you do need to understand why a change was needed and what was driving the change. This will help you understand how to move forward.
In the first post, I discussed the impact of how the brain works that leads to the development of an Opioid Use Disorder (OUD). I also discussed the issue of what was termed “Pseudo-Addiction” and how that concept led to prescribers and patients agreeing to higher and higher doses of pain medications. In this context, there was also the idea that our bodies could handle the higher doses and often “experts” in the field openly indicated that “there is no ceiling, we can go as high as the patient needs to go in order to control their pain.” This “no ceiling” rule led to people being prescribed massive amounts of opioids. I have seen it; people on 2,000 plus milligrams of morphine or morphine milligrams equivalent. Today we are going to discuss how those high doses proved to be fatal in some cases. I will also discuss why your body is not able to deal with unlimited doses of anything; it will impact us in more than one way.
Essentially what happened is shown in the graph below. We always knew that opioids are a respiratory depressant, which means that they have an impact on your body’s ability to breathe. Some in the field thought that as your body became more familiar with the dose, tolerance to that dose would occur and your body would be able to tolerate a higher dose, and your ability to breathe would not be impacted. Although that may happen at a lower dose, it did not occur sufficiently enough. In the end it was discovered that opioids at higher doses were leading to UNINTENTIONAL OVERDOSES for individuals taking their medication exactly as prescribed. Unfortunately, many people experienced these problems but it was not identified early on as directly due to the opioid. People were said to have died in their sleep from a “heart attack” or “unknown causes,” but in hindsight, the person was struggling to breathe or respirate, and that put a tremendous strain on their body. Sometimes, these people thankfully did not die and survived because they had a family member aware that they struggled with breathing at night, so they were watching them. They were saved from the one event only to continue on the medication that was causing the problem.
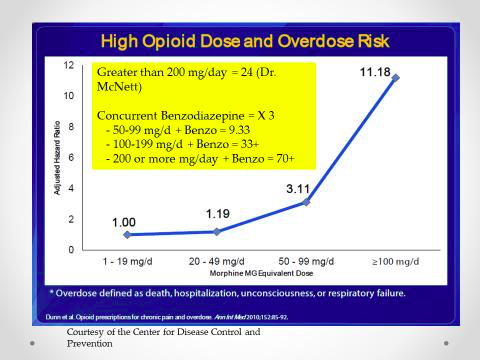
The graph above is a game-changer in understanding what was occurring and the true RISK of opioids being a factor in UNINTENTIONAL OVERDOSES. Before we jump into the graph, we have to understand MORPHINE MILLIGRAMS EQUIVALENT (MME). This is a concept where every opioid related pain medication is measured in terms of how “strong” they are in comparison to morphine. This is not just the strength of the opioid in terms of pain relief but balanced with the impact of the medication on respiratory depressant effect in comparison to morphine. A simple example is oxyCODONE products (e.g., OxyContin or Percocet). In terms of relative strength oxyCODONE products are 1.5 x stronger than morphine in terms of impact on a person’s ability to breath. So, 30 mg of oxyCODONE (or OxyContin) is equivalent to 45 mg of morphine.
As can be seen from the graph above, MME doses less than 50 MME had limited impact on the breathing and were identified as relatively safer or less likely to cause an UNINTENTIONAL OVERDOSE. Doses between 50-99 MME show a tripling of the risk for an unintentional overdose, while doses above 100 MME led to a massive increase. Doses > 200 MME led to another massive increase in risk. If we add in a benzodiazepines, which are medications that help manage anxiety and panic attacks (e.g., Alprazolam / Xanax, Lorazepam / Ativan, Clonazepam / Klonipin or Diazepam / Valium) then this fundamentally TRIPLES the risk of an unintentional overdose at every level. So a person on 60 MME and Alprazolam suddenly has a 9.33 overdose risk due to that combination.
A bit of perspective is needed here. The risk for an unintentional overdose for a person on 75 MME is 3.11, which is roughly equivalent to the risk of death associated with an untreated sleep apnea. Sleep apnea is a condition where the airway closes off during sleep leading to them stopping breathing while their body fights to open the airway by convulsing the diaphragm that is connected to the bottom of the lungs. This is similar to what we do when we perform the Heimlich Maneuver on a person who is choking on food, it compresses the lungs to push the air pressure up on the closed off throat (either due to food or the airway collapsing on itself). The key with this comparison is that UNTREATED SLEEP APNEA IS A MAJOR HEALTH RISK and it kills people. So, now we have prescribed a medication that is causing a major health risk for the patient.
What the Center for Disease Control and Prevention (CDC) determined is that the RISK that is caused by opioids on breathing (especially at night) is too great a risk to overcome the benefits when the dose goes above 90 MME. Further they indicated that when the dose is between 50-90 MME (or the person has other health factors that impact breathing at a lower dose) they need to be prescribed Naloxone (e.g., Narcan) to reverse the effects of an overdose if that should occur. Think about this a moment, we now have to prescribe a medication to REVIVE a person due to the effects of another medication that was prescribed. How crazy is that!
There is NO ARGUMENT against the basic facts here. Opioids, as the dose increases (or they are paired with other health conditions that influence ability to respirate or medications such as benzodiazepines) pose a major impact on the person’s ability to properly breath, especially at night while lying on our back or stomach when our ability to breath is much harder to begin with.
This is the story behind the SECOND factor that led to changes in the opioid prescribing guidelines. We do not know how many people died from this. We only know that people did die from this. Peoples lives were ended because they were taking a medication that was prescribed by their provider and likely were told that “this is safe.” Very scary situation.
The next post in this series will focus on why opioids do not continue to provide pain relief in the way they were intended to over the long haul. This will help you and your family understand why chronic opioids do not work the way we want them to work and why they may actually be making your pain WORSE. The concept of OPIOID INDUCED HYPERALGESIA will come into play here. Patients who see me, usually arriving to our pain clinic on massively high doses of opioids, will consistently say that this discussion is the most eye-opening discussion they have had about their pain or their pain medication. By the end of this discussion nearly 100 percent of my patients and their family members are motivated to reduce their reliance on opioids. Stay tuned for this post.
If you have questions or comments on these posts, please feel free to submit them at paindocblog@gmail.com. I would love to hear from you, learn from you and answer your questions in future blog posts. Remember that the opinions expressed in this blog are my own and do not necessarily represent those of Marshfield Clinic Health System.
